N-nitrosamines in Drug Products: Overview, Challenges and Lessons Learned from an API Manufacturer’s Perspective
By Karina Boszko, Head of API Regulatory Affairs and Customer Technical Support Department, Polpharma API
Nitrosamines—how has it all started?
In July 2018, the pharmaceutical industry was surprised by the unexpected detection of potentially cancer-causing chemical N-nitrosodimethylamine (NDMA) impurities in human medicines, which caused the recall of several drugs containing valsartan, used to treat high blood pressure and heart failure. A separate review was also started for ranitidine, alerting patients and healthcare professionals about exposure to unacceptable levels of this impurity. This initiated a discussion among health authorities and pharmaceutical manufacturers on possible risks of nitrosamines contamination. The valsartan case showed that nitrosamines were generated during the synthesis of the active pharmaceutical ingredient (API). The US Food and Drug Administration’s (FDA) review was followed by an EU-wide examination of the risk of nitrosamines in all human medicines. As a result, nitrosamines were detected in several other active substances, including metformin and rifampicin.
Nitrosamines, or N-nitrosamines, refer to any molecule containing the nitroso functional group. These molecules are of concern because nitrosamine impurities are probable human carcinogens, signifying that long-term exposure above certain levels may increase the risk of cancer development.
On September 26, 2019, the European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP) requested as a matter of precaution that marketing authorization holders (MAHs) for human medicines containing chemically synthesized active substances (APIs) review their drugs for the possible presence of nitrosamines. Based on EMA recommendations, the assessment should be performed in three steps:
Step 1: MAHs to perform a risk evaluation to identify if API and/or finished product could be at risk of the presence of N-nitrosamines. Deadline was until March 31, 2021 for human medicines containing chemically synthesized APIs.
Step 2: If a risk is identified, MAHs proceed with confirmatory testing to confirm or refute the presence of N-nitrosamines using validated and sensitive methods. MAHs should inform the competent authorities immediately if tests confirm the presence of a nitrosamine impurity irrespective of the amount detected.
Step 3: If the presence of N-nitrosamine(s) is confirmed, MAHs should implement effective risk-mitigating measures through the submission of variations. MAHs should apply for a variation in a timely manner to introduce any required changes, such as an amendment of the manufacturing process or changes to product specifications.
Steps 2 and 3 should be completed before September 26, 2022 for human medicines containing chemically synthesized APIs.
Similar recommendations have been published by the FDA.
The nitrosamine impurity issue extends beyond Europe and the US. Due to that, various regulatory authorities have partnered to share information, coordinate inspection efforts, and communicate effective analytical methods to detect and identify the risk of nitrosamines as well as to develop rapid solutions to ensure the safety and continuity of the drug supply.
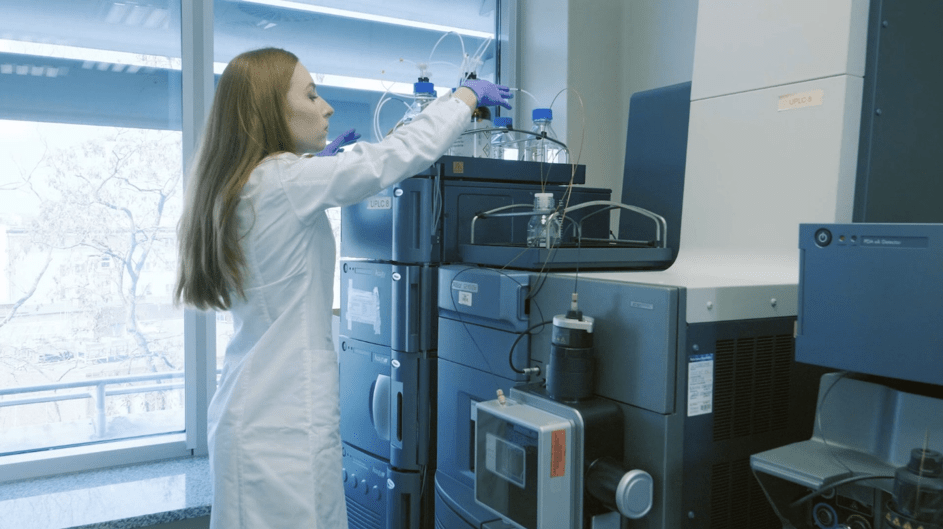
Being outside the pharmaceutical industry and hearing reports of valsartan and other products’ withdrawals, you might be wondering if nitrosamines are a new problem? Why has such risk not been spotlighted before? Already several years back, scientific literature reported nitrosamines as an impurity of several other drugs, thus underlining the apparent risk. Today, we have better testing methods than ever before. Moreover, we have much better equipment that detect impurities at extremely low levels. Currently, we know that we have to use GC-MS or GC-MS/MS due to its high selectivity and low detection levels. For example, in Polpharma, we use GC-MS/MS chromatographs with headspace autosamplers and UPLC-MS/MS chromatographs, which allow us to achieve a detection limit as low as 0.001 ppm. This improved technology enables us to detect even trace amounts of impurities in drug products. It may be why more products have been found to have low levels of nitrosamines. Moreover, regulatory agencies and pharmaceutical manufacturers know what to look for in products’ chemical structures and manufacturing processes that may increase the risk of forming low levels of nitrosamines.
Since the EMA and the FDA published their first guidelines, they have changed over time. Timeframes, the potential nitrosamines, sources of nitrosamines, and limits calculations have been continuously revised. All those actions have been implemented due to consultation with the pharmaceutical industry and growing knowledge of regulatory agencies and manufacturers on the nitrosamines subject.
Nitrosamines—potential sources
During ongoing investigations, it was also concluded that the possibility for nitrosamine impurity content was broader than simply the presence of nitrites and amines in the synthesis of the active pharmaceutical ingredient (API).
Polpharma, as an API manufacturer, has already completed three steps recommended by the EMA and the FDA, which means risk assessment and confirmatory testing. Thanks to our broad in-house experience and knowledge gathered during the last three years of the intensive work of a multidisciplinary team—chemists, analysts, regulatory affairs, process engineers—we know that there are many ways and conditions for the formation of nitrosamines in the API. The most common are: (a) the usage of nitrosating agents in the presence of secondary or tertiary amines within the same or different steps of the manufacturing process and (b) use of contaminated starting materials and intermediates supplied by vendors who use processes or raw materials that may contain residual nitrosamines or nitrosating agents.
Due to that, one mitigation strategy described in the FDA’s guidance includes a supplier qualification program that takes into account potential nitrite impurities across excipient suppliers and excipient lots to reduce the risk of nitrosamine formation in the drug product. An addition source of impurities is the use of contaminated recovered or recycled materials or certain packaging materials. The source can also be cross-contamination due to different processes being run successively on the same manufacturing line or carry-over of impurities between process steps and many others. Another source can be degradation processes of starting materials, intermediates and active substances, including those induced by inherent reactivity (e.g., presence of nitro, oxime, or other functionality) or by the presence of an exogenous nitrosating agent. Often formation of nitrosamine impurities lacks optimization of the manufacturing process for APIs when reaction conditions such as temperature, pH, or the sequence of adding reagents, intermediates, or solvents are inappropriate or poorly controlled.
We know it is not easy to find and understand the cause of the formation of nitrosamines. As our experience and knowledge grew along the way, we’ve updated the in-house risk assessment process and developed additional analytical methods to ensure our products’ safety. After these few years, we can confidently say that our knowledge of nitrosamines in APIs is extensive. The active substances produced by Polpharma have been thoroughly analyzed in terms of the risk of nitrosamines and tested with in-house developed and validated highly sensitive analytical methods. Following the recommendation of Step 3, we implemented changes to the manufacturing process, which reduced the risk of nitrosamines formation completely. The topic of nitrosamines is complex and requires deep multidisciplinary knowledge of experts from various areas. To face it, at Polpharma, we have created a team of our best technologists, analysts, regulatory affairs experts, and process engineers. Additionally, we bought top-class analytical equipment to develop very sensitive methods for testing our APIs. Despite the fact that all activities recommended by the EMA are completed, our team is continuously expanding its knowledge.
We are aware that potable water used in API production process may contain low levels of nitrite and even nitrosamines from environmental contamination. The existence of nitrites in processing water may lead to nitrosamine contamination in API production. Therefore, API manufacturers should analyze nitrite and nitrosamine levels in water and use purified water to remove unacceptable impurities.
We considered that more than 300 nitrosamines are currently known, many of which are highly potent mutagenic carcinogens; in some cases, N-nitroso-APIs can be formed. In August 2021, Pfizer voluntarily recalled some batches of Chantix (varenicline) tablets due to the presence of a nitrosamine, N-nitroso-varenicline, above the Pfizer established Acceptable Daily Intake (ADI) level. A similar case happened in October last year (2021); Lupin Pharmaceuticals Inc. voluntarily recalled batches of irbesartan tablets and irbesartan and hydrochlorothiazide tablets due to detected above the specification limit for the impurity, N-nitrosoirbesartan. There are some other cases of known N-nitroso-APIs that we have also entered into our risk assessment evaluation.
Sometimes it is challenging to evaluate mutagenic properties of identified nitrosamines. We also had such situations, and in case of any doubts, we used Lhasa software like Derek Nexus and Sarah Nexus. Additionally, in some other cases, Ames tests were performed.
The EMA and the FDA recommend that finished dosage form (FDF) manufacturers in their risk assessment collaborate with the API manufacturer to aid in identifying the API route of synthesis or other process conditions of the API’s production that put the drug product at risk for nitrosamine impurities. At Polpharma, being a vertically integrated company, we composed a group of experts in the field of API and FDF formulation, commonly working on risk assessment and evaluation. We believe the agency’s recommendation of close cooperation between FDF and API manufacturers should mitigate the risk of the presence of nitrosamines during the manufacture and storage of all medicinal products containing chemically synthesized APIs. That’s why we closely cooperate with our customers, sharing knowledge and experience.

Lessons learned and what’s next?
In June 2020, the EMA published an overview and recommendations as lessons learned from the nitrosamines experience. Even though the industry performs robust risk assessments to either discharge the risk or perform analysis to confirm/discharge that risk, we know there are still many ongoing challenges. Often manufacturers and regulatory agencies are still surprised by the results from testing their products.
The most important recommendation is to improve the exchange of information between Certification of Suitability (CEP) or Active Substance Master File (ASMF) holders and MAHs regarding impurity formation during API manufacturing, the manufacturing process and materials used in manufacturing so that MAHs can take full responsibility for the quality of their products, including APIs. Only through full cooperation and information exchange between MAHs and API manufacturers can the quality and safety of the drug be guaranteed. That’s why at Polpharma we provide our customers with access to data such as route of synthesis and information about contaminants from APIs to guarantee information exchange and full transparency with access to ASMFs, even when the CEP is available. The EMA also requires MAHs to include data on impurities and information from the API manufacturer in their dossier, irrespective of how the active substance documentation is submitted, e.g., via ASMFs or CEPs.
With respect to GMP guidelines, the EMA’s lessons learned group proposed to clarify regulatory expectations for technology transfers and supplier qualifications, clarify regulatory expectations for qualification and validation of facilities, equipment, utilities, and processes for active substance manufacturing and also ensure batch-specific supply-chain traceability between APIs and finished products.
As a lesson learned, regulatory agencies recommend that the network take steps to expand international collaboration with regulatory authorities around the world, including those in major exporting countries. Such cooperation immediately started when problems with the presence of N-nitrosamines in sartans appeared. It was clear from the beginning, that it would have immediate global implications. At that time, Health Canada created an ad hoc “Angiotensin II Receptor Blockers (ARB) International Strategic Group” to coordinate the various authorities’ activities and ensure that they were aware of each other’s actions. The strategic group comprised Health Canada, the EMA, the FDA, Japan’s Ministry of Health, Labour and Welfare/Pharmaceuticals and Medical Devices Agency, Australia’s Therapeutic Goods Administration, Singapore’s Health Science Authority, and Swissmedic. Areas of cooperation included the assessment of risks, testing methods and inspections, and public communication.
Nitrosamines can be eliminated by GMP, synthetic route modifications, elimination of nitrosamine formation sources, and a holistic understanding of the entire manufacturing process. As a result of growing knowledge about nitrosamines, some recommendation to process modification was published by regulatory agencies. The first of these possible mitigation strategies is derived from literature reports showing that commonly used antioxidants such as ascorbic acid (vitamin C) or alpha-tocopherol (vitamin E) inhibit the formation of nitrosamines in vivo based upon data from human gastric fluid in vitro studies. A second possible approach is based upon the fact that the formation of nitrosamines typically occurs under acidic conditions, whereas, in a neutral or basic environment, the kinetics of these reactions are significantly reduced.
And at the end, the case of nitrosamines showed an additional important point—with each news headline about the affected drugs, the public’s trust in the safety of their medicines deteriorated. Patients debated whether they were in more danger by taking their medication than they would be if they stopped. The patients were worried about the risk of cancer from drugs identified as having N-nitrosamines; many had concerns about alternative treatments. A recurring complaint from patients was a lack of clear information from regulators’ websites or healthcare professionals as to whether their own medicines were affected. Another lesson learned is implementing best communication practices and employing more communication tools (e.g., social media) to improve the content, clarity, presentation, timing, and dissemination of communication.
All this leads to the conclusion that science is constantly evolving. Expanding knowledge and experience combined with new technologies are the critical factors for the pharma industry’s evolution. Providing the highest quality and safe medicine is the most urgent part of the process in an industry where the most important is human health and life.
References:
EMA/409815/2020 Rev.7; Questions and answers for marketing authorization holders/applicants on the CHMP Opinion for the Article 5(3) of Regulation (EC) No 726/2004 referral on nitrosamine impurities in human medicinal products
EMA/425645/2020; European Medicines Regulatory Network approach for the implementation of the CHMP Opinion pursuant to Article 5(3) of Regulation (EC) No 726/2004 for nitrosamine impurities in human medicines
U.S. Food and Drug Administration: Updates on possible mitigation strategies to reduce the risk of nitrosamine drug substance-related impurities in drug products; Updates on possible mitigation strategies to reduce the risk of nitrosamine drug substance-related impurities in drug products | FDA
U.S. Department of Health and Human Services; Guidance for Industry: Control of Nitrosamine Impurities in Human Drugs
EMA/526934/2019; Lessons learnt from presence of N-nitrosamine impurities in certain medicines.
Author: Karina Boszko, Head of API Regulatory Affairs and Customer Technical Support Department, Polpharma API