Nanoform: Small is Powerful and Sustained – The Value of Nanoparticles in Sustained-Release Formulations
Introduction
Formulating small-molecule drugs for the parenteral route can offer important benefits over an oral delivery route, including faster onset of action, less room for error in emergency situations, and the ability to bypass a high first-pass effect and stability or absorption issues in the gastrointestinal tract.
Formulating biologics for a subcutaneous administration route instead of an intravenous one may allow a lower number of injections, or even substitute the need for long-time infusions administered at a hospital. The latter can necessitate frequent and costly hospital trips. This can have a cascading effect on compliance as patients struggle to keep appointments and follow treatment courses. To tackle this challenge, innovative solutions are required to enhance the efficacy and manufacturing of injectable therapeutics, therefore improving the patient experience.
Sustained-release parenteral formulations or implants that allow local administration of the drug are key to solving the major issues faced by patients prescribed injectable therapeutics. They can reduce the expense and time commitment for patients, improving compliance and positively impacting quality of life. Sustained-release implants can also enable improved local drug-delivery efficiency by concentrating the drug at the target site, thereby minimizing systemic exposure and resultant adverse side effects. These benefits are particularly felt by patients suffering from conditions with limited treatment efficacy, such as obesity, or which require drug application multiple times a day, such as glaucoma.
Taken together, it is clear that advances in sustained-release drug delivery could improve efficiency and consistency in drug release, manifesting in real-life advantages for patients in the form of enhanced accessibility and compliance.
Optimizing biologics for injection
The market growth in injectable drug delivery is largely driven by the increasing demand for large-molecule drugs, otherwise known as biologics. According to one report, these accounted for 51.8% of the market share for injectables in 2021, with their popularity largely driven by their potency, high selectivity, and related demand for biologics in the ever-expanding oncology sector.
Biologics are commonly formulated for the intravenous route, in large part due to stability and permeability issues that do not allow oral administration. This results in a need for frequent administration and poor patient compliance—an issue further exacerbated by the fact that biological therapies are more common for chronic diseases, which often necessitate lifelong treatment plans. Advances in sustained release formulations for subcutaneous administration of biologic drugs promise significant benefits for patients, including fewer hospital trips and improved compliance.
Nanoparticle engineering, a powerful technique that reduces the size of drug particles to the nanoscale, is well positioned to improve patient outcomes in the biologics space. Nanoform’s biologics technology can reduce the size of biological nanoparticles to as small as 50 nm, without negatively impacting stability. Nanosizing to this extent could enable increased drug load per unit volume for biological therapies, resulting in faster intravenous administration and increased comfort for patients.
Opportunities to enhance sustained-release implants In addition to increasing the drug load of injectable drugs to streamline administration, there is also a strong interest in long-acting implants with an enhanced drug load.
Ethylene vinyl acetate (EVA), a low-melting thermoplastic, is one material used to manufacture implants. Due to its compatibility with a wide variety of drug molecules and established manufacturing processes – such as hot-melt extrusion and co-extrusion—EVA implants are well established for long-acting cutaneous delivery with multiple approved drug products.
However, there remain opportunities to further optimize EVA long-acting implants and increase drug load. One persistent challenge in the industry is that at high drug loadings, monolithic implants exhibit a high initial burst release and greater than desired overall release rate.
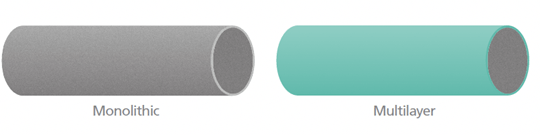
The standard solution used by multiple marketed products is to produce multilayer implants via coextrusion. These consist of a highly-loaded core with a rate-limiting outer layer—this layer reduces the burst release and can be used to tune drug-release kinetics in a manner that is independent of drug loading in the core. However, there are cases where designing a multilayer implant is inconvenient. For example, non-cylindrical implants are often best manufactured via injection molding, which would require additional manufacturing steps to apply a rate-limiting layer to an implant. As a result, there is a strong need for alternative methods to optimize drug-release kinetics.
Game-changing research on optimizing sustained-release implants
A study led by Nanoform, an innovative nanoparticle medicine-enabling company, and Celanese, a global specialty materials company, sought to clarify the effect of drug-particle size on drug-release kinetics from highly-loaded EVA implants. In highly-loaded monolithic implants, drug release occurs through a network of pores created by dissolved drugs. Changing particle size alters the polymer—drug physical interactions and was expected to impact drug release kinetics.
The research leveraged Celanese’s VitalDose® EVA copolymer delivery technology for drug-eluting implants and Nanoform’s game-changing Controlled Expansion of Supercritical Solutions (CESS®) technique. The latter dissolves and recrystallizes bulk API powder under carefully controlled temperature and pressure to create drug substance nanoparticles as small as 10 nm in some cases. In this study, CESS®-produced nanoparticles of two potent drugs, risperidone and fingolimod, exhibited a slower release rate in EVA implants relative to bulk material.
Nanoformed risperidone also exhibited a much lower initial burst release than micronized risperidone, which was tested as the control. The results demonstrated the exciting potential of CESS® nanoparticle engineering as an alternative method to solve the long-standing challenge associated with the drug release kinetics of implants for long-acting subcutaneous delivery.
Manufacturing a superior implant
Nanoforming has shown its power for solving the long-standing challenge associated with sub-optimal release kinetics in long-acting implants, but it doesn’t end there—the benefits carry along further into the manufacturing stages.
Reducing API particle size down to the uniquely small nano-size range that Nanoform is able to achieve could facilitate smaller implants with increased drug load, enabling lower polymer content, smaller drug products and devices, smaller packaging, reducing logistical burden and improving carbon footprint in supply chains.
Small is a game-changer in sustained release
From treating ocular disorders to obesity and more, there is a clear, patient-driven need for enhanced long-acting implants that can improve quality of life. Cleverly designed sustained release implants leveraging Nanoform’s advanced nanoparticle engineering technology could possess a higher drug load in a smaller-sized package, offering important manufacturing and patient benefits that will lead to better therapeutic outcomes.
Discover why small is powerful for sustained-release implants in our most recent case study, “Using Drug Nanoparticles to Modify the Release Kinetics of Ethylene Vinyl Acetate Long-acting Implants.“
Alternatively, contact us at info@nanoform.com to discover how we can enhance your drug development projects.